Latest News & Stories
Get the latest from the Endowment and read more about the impact of the work being done by our grantees and individuals in the field
News / Story


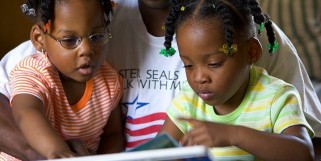
Church-based Literacy Camps are Filling a Gap in Summer Learning
How church-based literacy camps are filling a gap in summer learning for rural students statewide.
July 23, 2025 | Kristen Richardson-Frick, Mebane Rash and Hannah Vinueza McClellan